Focus On: Keratoconus
Keratoconus is a condition in which the cornea of the eye is “cone shaped”. A normal cornea has a smooth, regular curvature which resembles a section of a sphere or, in cases of astigmatism, somewhat the shape of a spoon. The keratoconic cornea with its cone-like bulge has an irregular shape, and in its moderate to advanced states causes blurred, distorted vision which cannot be properly corrected by regular glasses.
 Keratoconus is a non-inflammatory condition, and is usually caused by a progressive thinning of the central corneal tissues. Occasionally it may have other causes such as improperly fitting hard contact lenses. The etiology of the corneal thinning is not known, though in some cases it appears to be hereditary. Keratoconus usually occurs in both eyes, though one eye may be more affected than the other.
Keratoconus is a non-inflammatory condition, and is usually caused by a progressive thinning of the central corneal tissues. Occasionally it may have other causes such as improperly fitting hard contact lenses. The etiology of the corneal thinning is not known, though in some cases it appears to be hereditary. Keratoconus usually occurs in both eyes, though one eye may be more affected than the other.
Keratoconus is a relatively rare condition, and is said to afflict less than 1 person out of 2 thousand. However, because the severity of keratoconus varies greatly, milder cases are not always diagnosed. The condition normally begins after puberty and may progress slowly over of a period of many years.
Keratoconus is suspected when frequent changes in glass prescription, requiring more correction for near-sightedness with a marked increase in astigmatism, are necessary and the maximum visual acuity diminishes even with the best prescription.
The condition may be easily diagnosed by using instruments such as the keratometer, which measures the central corneal curvature. As the condition progresses the curvature readings become steeper and begin to appear irregular. The peripheral corneal shape and curvature can also be measured by various methods such as corneal topography, which measures corneal shape, to ascertain the size and the configuration of the cone.
Our doctors at Vision Care Consultants are nationally recognized experts in keratoconus and are on the National Keratoconus Foundation’s (NKF) referral list of doctors.
Because the corneal surface of a keratoconic eye is distorted and irregular, the best visual acuity can only be achieved by replacing it as the primary refractive surface. This can usually be achieved by covering the corneal surface with a contact lens or replacing its central section with a corneal transplant supplied by a donor. Refractive surgery techniques such as LASIK are contra-indicated in cases of keratoconus, because they do not work well when used on thin irregularly shaped corneas and even make the keratoconus worse.
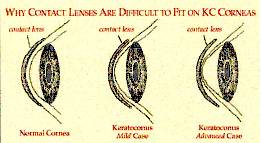
When contact lenses are used, hard lenses are the lens of choice. Soft lenses are thin and flexible, following the contour of the eye, and are usually not effective when used as a correction for keratoconus. Occasionally, soft lenses are used in conjunction with hard lenses which are “piggy backed” on top of the soft lens surface.
The preferred materials for use in fabricating hard lenses is usually a gas permeable plastic which permits oxygen to pass through the lens and therefore helps maintain the normal metabolism of the corneal surface. These lenses must be custom made to provide the optimum fit over the irregular corneal surface of a keratoconic cornea. In some cases, if properly fitted, they may help also to retard the progression of keratoconus by putting a “cap” on the top of the cone. Unfortunately, the recent advances in the plastic used for lenses are not always combined with the best in custom fitting, and many contact lens wearers with keratoconus suffer unnecessary discomfort and sometimes even the inability to wear the lenses that they depend on for normal vision.
Advanced keratoconus may result in corneal scars and opacities which may lead to the need for a corneal transplant. It is important that the transplant be performed before the area surrounding the central cornea becomes too thin.
All told, approximately 10,000 corneal transplants are performed each year in the United States for various conditions, including keratoconus. Corneal transplant surgery is an art as well as a science, and it is important that those seeking such surgery find an experienced and successful surgeon. When performed properly, the surgery is relatively non-traumatic, and is over 90% successful. After the surgery many keratoconus patients experience normal vision, though most will require the additional use of contact lenses or glasses.
Corneal Collagen Cross-Linking
A new procedure, corneal collagen cross-linking (CXL), is now available for keratoconus. This non-invasive procedure is performed with vitamin eyedrops and a special wavelength of light. CXL’s purpose is to strengthen the cornea, prevent further deterioration of vision, and potentially help keratoconus patients improve their vision.
In 1998, doctors in Germany introduced CXL with riboflavin eyedrops and UV light to treat patients with keratoconus. Today, doctors are performing CXL and successfully treating patients in over 400 centers outside the United States, including all 25 European Union nations since 2006. This treatment is not yet widely available in the U.S. because the Food and Drug Administration (FDA) has not approved the use of UV light and riboflavin in this therapy. Through a research study, Vision Care Consultants is now able to offer this investigational treatment to our patients using advanced technology for cross-linking.
Normal corneas have cross-links within their collagen fibers that keep it strong and able to retain its normal shape. In keratoconus, the cornea is weak, with too few cross-links. This weakened structure allows the cornea to bulge outwards into irregular shapes, which causes poor vision, glare and difficulty seeing. The cross-linking procedure adds cross-links to the cornea, making it more stable, holding its shape and focusing power better. These new cross-links help strengthen the cornea, which stops the thinning process and further loss of vision.
To qualify for CXL, patients must be at least 12 years old and their corneas cannot be too thinned or too scarred for the procedure. Our doctors can determine if CXL might be an option for you.
The CXL treatment is an outpatient procedure performed using numbing eye drops and a mild sedative. Before the light is used, the epithelium, a thin layer of clear, protective tissue (like skin) that covers the cornea is prepared for the CXL procedure. Next, vitamin B2 eye drops (riboflavin) are used in the eye and the patient is asked to look at a special blue (ultraviolet) light while lying comfortably on the reclining chair. It’s generally easy for patients to look at this light because the eyes are numb and drops are used to keep the eyes moist. From a patient’s perspective, the UV light appears to have a soft blue color. The crosslinking procedure is painless, as anesthetic eye drops are used to avoid discomfort. If two eyes are being treated at once, the procedure takes approximately an hour and a half. If only one eye is being treated at a time, the procedure takes approximately one hour.
In the least invasive CXL treatment called transepithelial (or epi-on) CXL, the surface skin layer (epithelium) of the cornea is not removed so the recovery is much faster than the traditional CXL technique. This least invasive technique can only be done on corneas that are thick enough. The surgeons that Vision Care Consultants have partnered with perform only the transepithelial technique. With transepithelial (or epi-on) CXL, most people return to their usual activities the next day and contact lens wearers can typically return to wearing contact lenses within a few days to a week.
The main purpose of CXL is to prevent further vision loss and the need for future corneal transplant, as it is a mainly preventive treatment. However, some patients also get some improvement in their vision as well. Generally, with CXL, visual improvement is a long process. Some patients have found their vision improved somewhat as early as several weeks after treatment; in some studies, patients’ vision was still continuing to improve five years after the crosslinking procedure. Many research studies have shown that CXL may prevent further vision loss in over 98% of patients treated. Because cross-linking can improve vision over months and years, patients often find that their old contacts or glasses are too strong for them and they need to be refit with new glasses and/or contact lenses.
As with most conditions, prevention of a problem is better than treatment of a problem. The best time to treat keratoconus is before the effects become apparent and vision has been lost. However, this does not mean that people with very poor vision from keratoconus cannot be helped by CXL. Make an appointment with one of our doctors at Vision Care Consultants to have your eyes checked and talk about whether CXL is an option for you.
